Background
Gastric and gastroesophageal cancers are common and carry an exceedingly high mortality rate. Of patients treated with curative intent, the majority have locally advanced disease, and require chemotherapy before and after radical surgery. Since 2017, 5-fluorouracil, leucovorin, oxaliplatin and paclitaxel (FLOT) based chemotherapy is the most commonly used perioperative regimen.
Tumour regression grade (TRG) is a histological method of assessing and classifying a tumour’s response to preoperative chemotherapy. However, whether TRG correlates with patient survival remains controversial. This is particularly so in the era of FLOT-based chemotherapy, where there is currently a paucity of data to guide clinical practice.
Additionally, to date, the role of TRG as a therapeutic biomarker for FLOT-based chemotherapy has not been evaluated. Based on clinical trials, 40% of resected gastric and gastroesophageal cancers demonstrate minimal or no response to preoperative FLOT-based chemotherapy. Furthermore, 20% of tumours exhibit complete pathological regression. Whether these two cohorts of patients derive further benefit (or harm) from postoperative FLOT-based chemotherapy requires clarification. It stands to reason that in cancers which do not respond to one specific treatment, administering more of the same in the postoperative period is potentially futile and harmful. Conversely, in patients with no residual disease, additional postoperative chemotherapy may be unnecessary.
Anecdotally, a lack of evidence to guide decision-making in this area has resulted in variations in practice. This includes continuing with more FLOT-based chemotherapy, withholding additional treatments, changing therapeutic regimens, or prescribing (chemo)radiation. To date, patterns of care in the postoperative setting for patients with complete pathological response, and those with minimal or no response to preoperative FLOT-based chemotherapy is yet to be described.
Aim
To audit the patterns of care and survival outcomes of patients with gastric and gastroesophageal adenocarcinoma who have undergone preoperative FLOT-based chemotherapy and radical surgical resection stratified by pathological response in the resected specimen.
We will address the following clinically relevant questions: In patients with gastric and gastroesophageal cancers who have undergone preoperative FLOT-based chemotherapy and radical surgery:
Does pathological response in the resection specimen predict patient survival?
What are the international patterns of care for patients with complete pathological response (pCR) and minimal/no pathological response (TRG3/4) to preoperative chemotherapy in the postoperative setting?
What are the clinicopathological predictors of tumour regression
Does the cohort with pCR benefit from further postoperative FLOT-based chemotherapy?
Does the cohort with minimal/no response benefit from further postoperative FLOT-based chemotherapy?
Patient Eligibility
Any patient with gastric and gastroesophageal cancer
Received preoperative FLOT-based chemotherapy and surgical resection between 01 January 2017 to 01 January 2022
Age ≥18 years-of-age
Study Design
This study is an international retrospective analysis of practice and outcomes between 01 January 2017 to 31 Dec 2022. Data collection will be through REDCAP database.
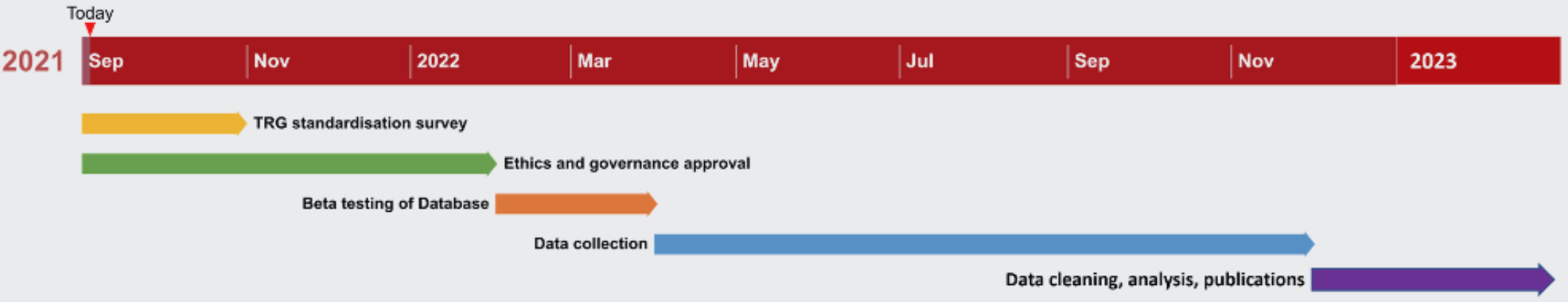
Project Timeline